Book an Appointment
Call Us+91 9319488481The brain, the central organ of the nervous system, is responsible for regulating cognition, movement, sensation, and emotion. Beyond its fundamental functions, it possesses a unique and powerful capability—neuroplasticity—the ability to reorganize, adapt, and heal itself in response to injury, learning, or environmental changes.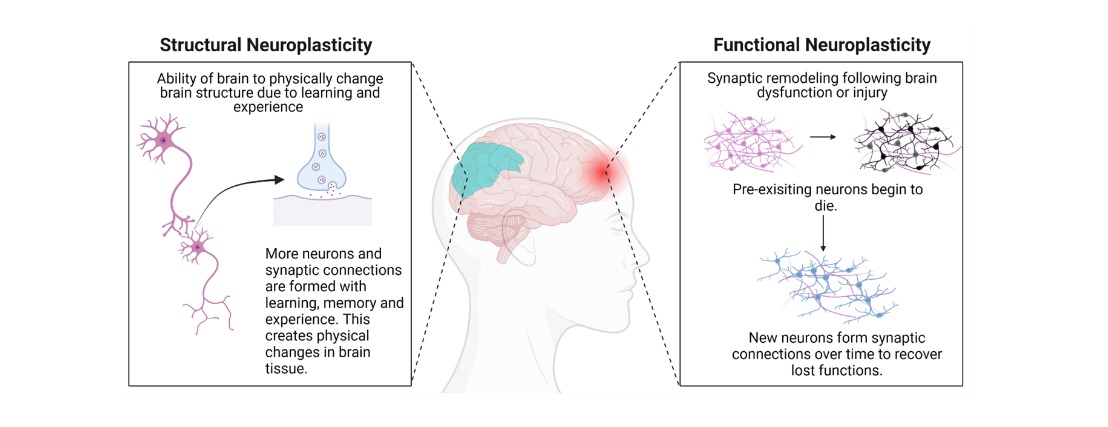
Neuroplasticity, also called brain plasticity, refers to the brain’s ability to reorganize itself by forming new neural connections throughout life. It allows neurons (nerve cells) to compensate for injury and disease and to adjust their activity in response to new situations or changes in the environment.
In clinical terms, neuroplasticity is the foundation for functional recovery after neurological injury.
Read Also: How Neurorehabilitation Helps in Stroke Recovery
The brain contains billions of neurons that communicate through synaptic connections. Repeated behaviors, thoughts, or physical activities strengthen specific neural pathways, enhancing efficiency and performance.
In cases of injury—such as ischemic stroke or traumatic brain injury—undamaged brain regions can assume functions of the impaired areas by forming alternative pathways, allowing partial or full functional recovery through compensatory mechanisms.
Read Also: Stroke Treatment and Rehabilitation: What Every Patient Should Know
This is the brain’s ability to transfer specific functions from a damaged region to undamaged areas. It's critical in post-stroke rehabilitation where speech or motor function is gradually restored.
This involves actual changes in the physical structure of the brain, such as synaptogenesis (formation of new synapses) and neurogenesis (formation of new neurons, primarily in the hippocampus).
Read Also: Effective Speech Therapy Techniques for Stroke Patients
Neuroplasticity is integral to rehabilitation medicine. With the appropriate therapy, the brain can regain lost functions after:
Yes. While neuroplastic potential is higher in early developmental stages, adults retain the capacity for neuroplastic change. Interventions in later life—such as cognitive training, aerobic exercise, and social engagement—can foster plasticity and reduce cognitive decline.
Following cerebral infarction or hemorrhage, the brain undergoes spontaneous plasticity within the first weeks, making early intervention critical.
Key Interventions:
Timeframes vary based on the severity of injury, type of intervention, and consistency. In clinical recovery, measurable changes may be observed within weeks to months, particularly with intensive and repetitive therapy.
Yes. Conditions like depression, anxiety, and PTSD are associated with maladaptive neural pathways. Treatments like CBT, EMDR, and mindfulness-based interventions promote adaptive rewiring and improve emotional regulation.
Children exhibit high levels of plasticity, enabling rapid language acquisition, motor learning, and resilience following injury. Early stimulation through play, education, and social interaction supports optimal brain development.
Yes. Despite its capabilities, neuroplasticity has constraints:
Neuroplasticity is a central principle in modern neuroscience and rehabilitation. Whether recovering from a neurological event or enhancing brain health, neuroplasticity provides a scientific foundation for hope and healing. With structured therapy and consistent mental and physical stimulation, the brain can rewire itself in profound and meaningful ways.
Q1. Can adults really change their brains?
A: Yes. Adult neuroplasticity is well-established in neuroscience. While changes are slower than in childhood, they are entirely possible.
Q2. How long does it take to develop a new neural habit?
A: On average, 21 to 66 days of regular repetition can induce durable changes in neural pathways.
Q3. Does neuroplasticity stop with aging?
A: No. It declines with age but persists throughout life. Cognitive and physical stimulation help maintain it.
Q4. Can neuroplasticity cure Alzheimer’s disease?
A: No, but it can delay symptom progression and support compensatory strategies for improved quality of life.
Q5. Is sleep essential for neuroplasticity?
A: Absolutely. Sleep is critical for synaptic pruning, memory consolidation, and neurorestoration.